Transforming Elective Orthopaedic Care for a Local Health Network in South Australia
A Local Health Network in South Australia transformed their orthopaedic service by bringing teams across two hospitals together to develop a best practice “one service, two sites” model.
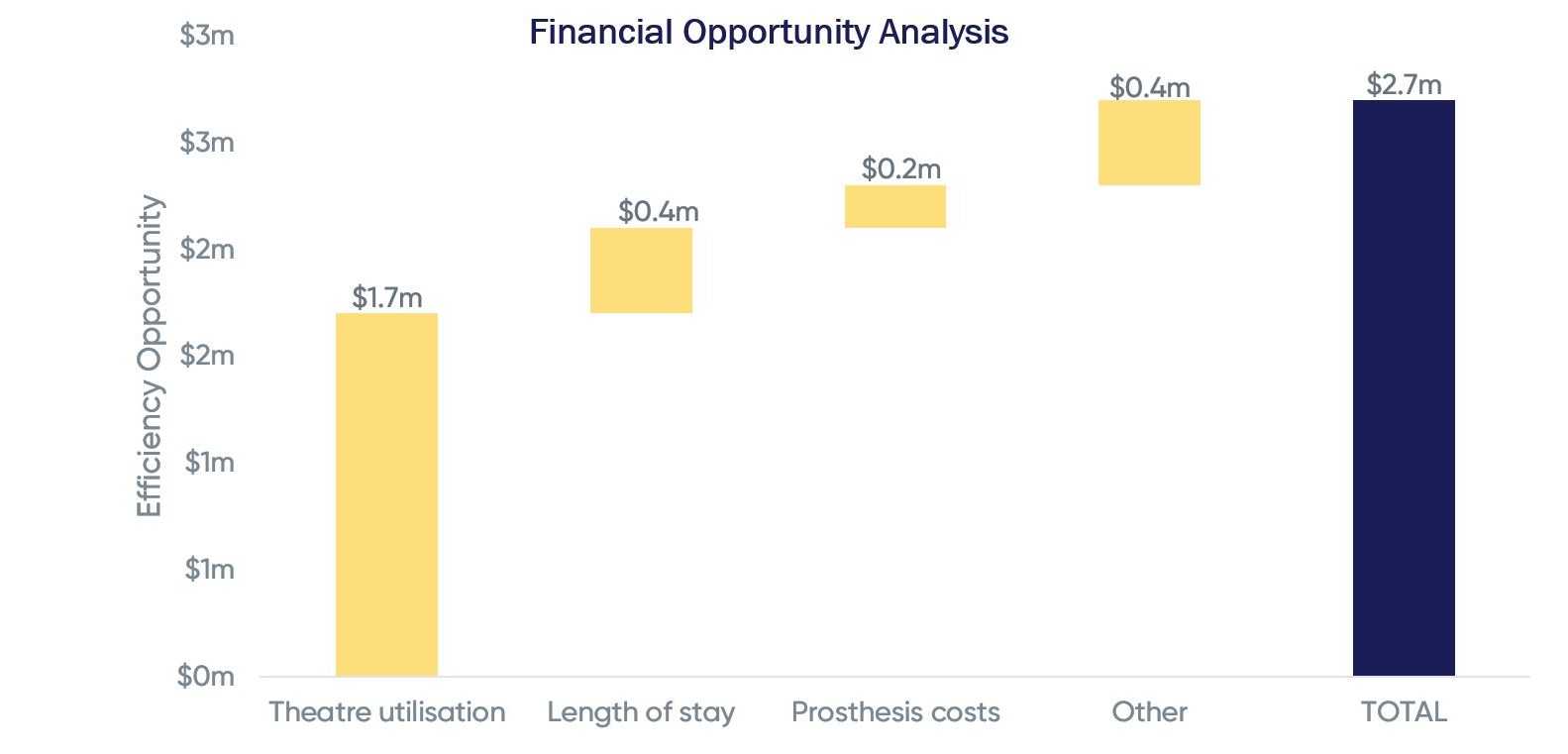
When we were brought on board, the service was operating in a challenging financial environment, providing services to an ageing population with increasing comorbidities whilst state funding projections remained flat. The Local Health Networks’s elective orthopaedic services were operating at a deficit of $4.8m (-20%), with overall service costs at 121% of national average (NEP).

What did we do?
Working with a multidisciplinary clinical leadership team across both sites, we facilitated the development of a shared vision for orthopaedic services to unify the two teams. We produced a roadmap for the design and implementation of a common best practice pathway and site configuration model that would capitalise on the teams’ expertise and combined scale. We drew on our knowledge of international best practice and complemented this with a targeted analysis of activity, finance, operations and outcomes data to identify the changes that were needed to achieve financial sustainability. The local multidisciplinary team were engaged through a series of clinical planning workshops, interviews and smaller group sessions, through which a holistic, preventative, patient-empowering model of care was established.
What’s been achieved?
This work delivered a common best practice pathway for high volume arthroplasty across both sites, and a phased approach to site reconfiguration to concentrate non-complex elective orthopaedic procedures at one site, and complex procedures at the other.
Common best practice pathway
Through the clinical engagement process and drawing on the best practice presented, the local team agreed to harmonise arthroplasty pathways across sites and to pursue key service changes including rolling out preoperative conservative management across both sites, engaging primary care, introducing a single point of referral across both sites and involving MSK practitioners in the triage process to significantly reduce referrals to orthopaedic surgeons.
Optimised site configuration
Through the planning process, the local team and Executive evaluated site options and agreed a future state model. This model enables the consolidation of routine procedures at the lower acuity site, where occupancy levels are lower and ringfencing of elective orthopaedic beds can be maintained to enable lower cancellation rates and more efficient scheduling. Complex procedures are consolidated at the specialist centre, co-located with the Major Trauma Centre, ensuring access to the most specialist and high intensity care available to achieve the very best surgical and health gain outcomes. Activity segmentation and capacity modelling was developed in close consultation with clinical leads to quantify the resulting bed and theatre requirements to accommodate the future state model.
Anticipated benefits
The common best practice pathway is expected to improve the health and wellbeing of people with joint pain in the community, supporting them to live healthy independent lives. The new site configuration and operating model lends itself to much improved operational efficiency. Collective anticipated productivity improvements are worth an estimated $1.7m per annum, bridging around 2/3rds of the gap to the state average NEP.
The PSC Australia Team