27/08/2021
Transformation, News, Insights
What will Amanda Pritchard do next?
As Amanda Pritchard's first full month as the new CEO of NHS England comes to a close, one of the first questions likely sitting on her desk is whether she will scrap the four hour standard - Eleanor Gibbon considers what will inform her next move.
With a pilot of 14 hospitals testing potential replacements coming to a close, and results of the public consultation have been released, the question of whether to scrap the four hour standard will be looming large for Amanda Pritchard.
Amanda has inherited a significantly different NHS from that of her predecessor. How can she consider whether the 4-hr standard, 2004's flagship target, is still a priority today?
The consultation and pilot schemes will provide good information, but to make a call on this issue, we think it's worth looking at three more areas:
- Worsening of external issues affecting performance
- The rise of new objectives
- Changing distributions of activity across the health and care system

Read our last piece on why it's time to move on from the four hour emergency department standard.
Changing distributions of activity across the health and care system
One of the central benefits of the 4-hr standard has been that in addition to indicating performance in Emergency Departments (EDs), it has been a useful proxy for performance across the health and care system as a whole. However, this may become less true with time, due to ongoing shifts in how activity is distributed across the system. As demand moves around, we may need new indicators to understand how well that demand is being managed.
Changing population health needs, including the impact of COVID, are a major driver of this shift. Further our ageing population, and the complex, long-term conditions that are now more common, are better managed in community rather than acute settings. This is leading to a greater increase in demand for long-term support relative to emergency care.
The balance is likely to tip further as demand for COVID aftercare and support falls on community health services, primary care, and mental health providers. Additionally, as the non-COVID elective backlog is tackled, there will be a surge in demand for post-surgical rehabilitation and discharge services.
These changes in the balance of activity away from ED suggest that ED performance may not remain a good barometer of health system performance. This was reflected in responses to the public consultation, where 80% of respondents said that "a bundle of measures would be more helpful than a single measure to understand how well an urgent and emergency care system is doing".
Amanda will need to consider how to future-proof the targets she selects, for example by focussing energy on collecting better national data from community services, primary care and mental health settings.
Worsening of external issues affecting 4 hr performance
We know that practically 4-hr performance is affected by a huge range of factors - some relating directly to EDs (e.g. staffing, operational efficiency), some relating to other parts of the hospital (e.g. bed occupancy, discharge processes) and others related to the wider system (e.g. demand, availability of alternative services). Recently, there has been a rise in systemic issues that sit outside of EDs, against which the 4-hr performance standard needs to be contextualised.
How do we know this? Our analysis of 4-hr performance shows that, after a drop in attends during COVID (and corresponding boost in performance), whilst ED attends have bounced back, performance has dropped below pre-COVID levels - the system appears to have been weakened.
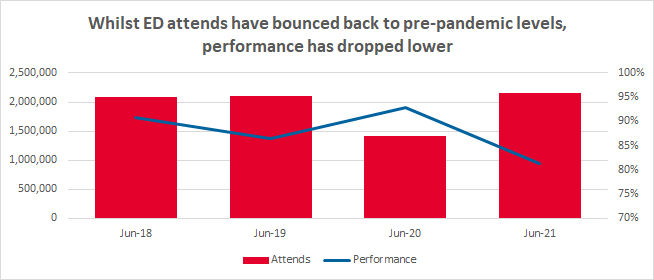
Currently, every region is performing below the 95% target, with 6 out of 7 regions showing performance below 90%. The likely root causes of this include workforce shortages, unprecedented demand for beds, and growing regional disparity - factors which largely sit outside of EDs' control.
To begin with workforce - a strong workforce was a key supporting element in the introduction of the 4-hr standard. It was accompanied by rapid increases in both spending and staff to facilitate improvement. However, as COVID-19 hit England last year, the health service faced workforce shortages of over 100,000 staff, around 40% of which was in nursing. Influences such as Brexit have made it particularly difficult to repair this shortfall. Any plan to reduce waiting times should incorporate an enabling workforce plan, to avoid overly-penalising remaining (burned-out) staff.
COVID-19 has also caused unprecedented demand for beds, which reduces the speed at which patients who need emergency admission can be admitted, and hence performance against the 4-hr standard. Unprecedented bed demand is likely to continue, although hopefully at a lower level, as the backlog in elective care is tackled. This task will likely require more beds to be ring-fenced for elective care, so 4-hr performance may not return to pre-pandemic levels for a number of years.
The PSC's analysis also shows that there is greater regional disparity in terms of 4 hr performance now than there was pre-COVID. The South-East region remains the highest performer, with performance in the lowest-performing region, the North West, approximately 8.5% lower.
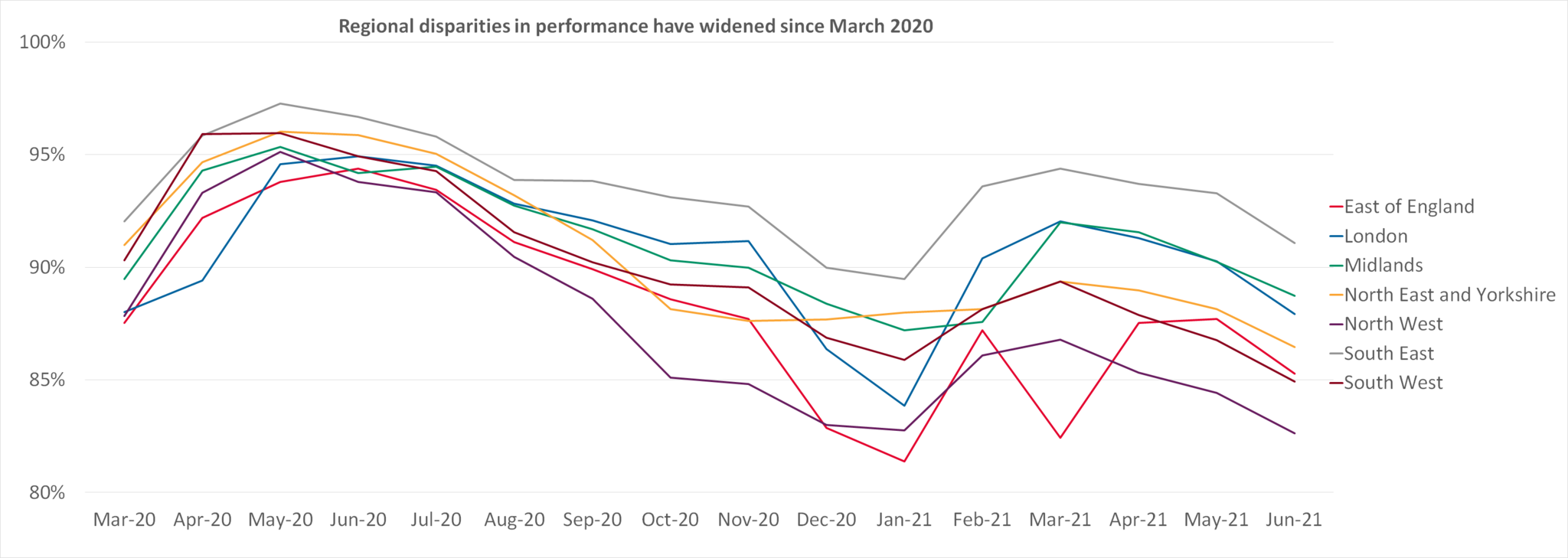
The causes for the growing disparity are not yet clear - the North West and South East have both been hit hard by COVID, taking 2nd and 3rd place for most COVID cases in the UK as of August 2021, behind London (Statista).
What does this mean for how the 4-hr standard might be used? Under Simon Stevens, performance data was used to distribute financial penalties to under-performing Trusts. However, if the causes for underperformance increasingly sit outside of EDs' control, is this still the right policy post-2021? Instead, Amanda might decide to lend support to under-performers rather than penalties - this would be more in-line with the government's levelling up agenda.
The rise of new objectives
Amanda is likely to soon publish her own objectives for the NHS, setting its strategic direction under her leadership. These may not be aligned with investing a lion's share of resource into improving 4-hr performance - if so, scrapping the target would encourage the system to "move on" from the old ways of thinking. Recently, key NHS objectives have also included the transition to net zero, reducing health inequalities, better service integration and population health management. Amanda might consider choosing a new flagship target that better reflects her new priorities.
A final thought
Deciding which target(s) to use is far from the end point. Amanda will need to consider what might drive the success or failure of her chosen target(s), and how she can use her role as leader of the NHS to cultivate success. Other questions that need consideration:
- How prominently should targets feature in her priorities, given the resource required to use them well? What might be the opportunity costs of this decision?
- How can she ensure any targets work to empower, rather than demoralise, exhausted staff?
- Which problems or perverse incentives might new targets generate, or solve?
- What data is needed to contextualise performance metrics?
- What might be some early warning signs of target gaming?
Although the public consultation response was positive, without a full review of the benefits and disadvantages of the ongoing pilot programmes, the jury is still out on what Amanda's next move should be.
What we can say, though, is that contextualising 4-hr performance against other factors is becoming more crucial than ever before. Whilst measuring how quickly people are treated, admitted and discharged in ED will always remain important, Amanda will need to consider the role of this metric in a permanently changed health and care landscape, and under her new leadership.
Author: Eleanor Gibbon, The PSC Transformation Team
Latest News & Insights.

Synthetic Research is Happening – Here’s What’s Out There
AI-powered synthetic research is moving fast. Here’s how public service…

The PSC and Parkinson’s UK Shortlisted for The 2026 HSJ Partnership Awards
Our Time-Critical Medications Dashboard has received recognition from The 2026…

Fit for the Future: Realising the ‘Left Shift’ from Hospital to Community
Insights from The PSC’s roundtable on community health, innovation and system…

